- Reduced risk of infection
- Access to anterior targets
- Acceptable, tolerable pain levels under local anesthesia
- Compatible with no antibiotic prophylaxis
- Provision of more cancerous materials for pathology
- Improved detection of clinically significant prostate cancer
- Identical orientation to focal therapies conducted via the perineum
Transperineal biopsies can be performed using a standard TRUS approach (blind) or an MRI/US fusion approach.
“Blind” Transperineal Biopsy
The 2D ultrasound image enables the urologist to navigate the prostate and spread out the biopsies (generally 12 biopsies, 6 per prostatic lobe) according to a sextant pattern in order to maximize their effectiveness.
The random nature of this method is such that the presence of significant cancers cannot be excluded.
Consequently, this substandard approach is characterized by inadequate, uncertain diagnoses that contribute to overtreatment and undertreatment.
MRI/US transperineal fusion biopsy
A precise diagnosis is essential to determine the best treatment pathway.
The use of MRI to detect prostate cancer represents the latest revolution in prostate cancer diagnosis. Prior to its development, ultrasound probes were only used for guidance, as they are limited to organ contour imaging, not the tumor within.
Prostate fusion biopsy is a revolutionary technology made possible by overlaying ultrasound images of the prostate with MRI sequences for visualization and targeting of lesions. Suspect areas detected by the MRI are thereby displayed on the ultrasound scanner, allowing the urologist to target the necessary biopsies.
This approach to prostate diagnosis and care has significant benefits for clinical teams and patients, eliminating the randomness of standard TRUS prostate biopsies.
Expect better patient outcomes with KOELIS Trinity® Perine
With 15 years of experience in targeted 3D transrectal US prostate biopsy, KOELIS® offers a freehand and stabilized transperineal approach.
KOELIS Trinity® is a versatile, all-in-one solution providing accuracy and reliability at every stage of the prostate cancer journey, from biopsy and active surveillance to treatment and follow-up.

At KOELIS, we specifically perform Elastic MRI/US Fusion, meaning the MRI is actually adapted to perfectly match the ultrasound, taking this fusion to a new, higher level of accuracy.
We have developed the only fusion technology that tracks the prostate itself, instead of the probe. This technology, called OBT Fusion® (Organ Based Tracking Fusion®), is what makes the KOELIS® solution unique.
Our 3D transducers combined with OBT Fusion® technology detect the slightest patient movement and prostate deformation for accurate guidance and recording of the procedure.
Using KOELIS Trinity®:
- Reduce patient discomfort during the procedure ¹, ² The KOELIS 3D motorized probe renders complete visibility of the whole prostate, even the largest prostates, without moving the probe, providing accuracy and comfort.
- Significantly reduce post-biopsy infections ¹, ²
- Improved detection of clinically significant cancers ¹, ², ³
- Provide the best possible care ³
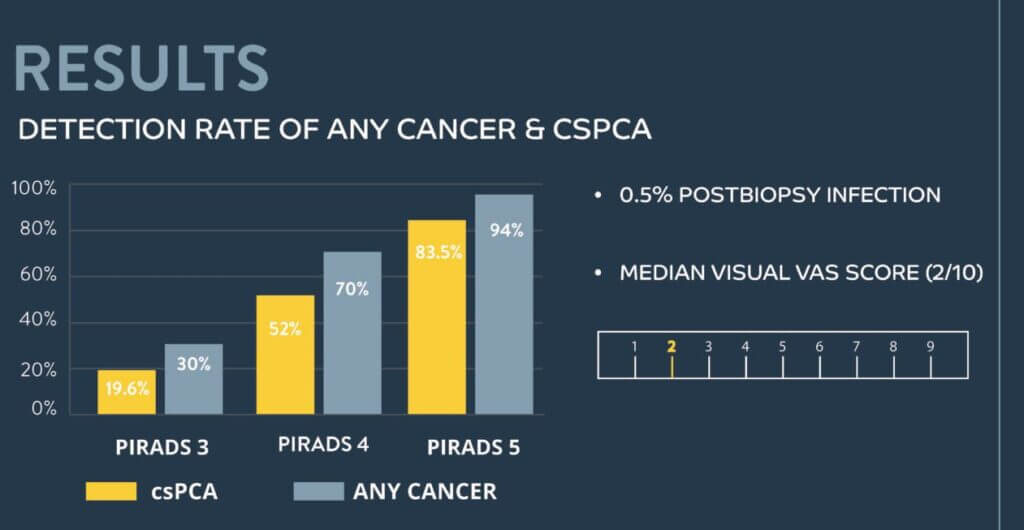
KOELIS study:
Multicenter transperineal MRI-TRUS fusion-guided outpatient clinic prostate biopsy under local anesthesia – Jacewicz et al. INT J UROL, July 2020
The KOELIS Trinity® has set a new standard in prostate fusion biopsy accuracy and reliability. As a result, it is the system of choice in many of the world’s leading centers.
More information on our prostate biopsies, needle guides and grids
Publications:
- (1) Multicenter transperineal MRI-TRUS fusion guided outpatient clinic prostate biopsy under local anesthesia – JACEWICZ et al. INT J UROL, July 2020
- (2) Infection rate and complications after 621 transperineal MRI-TRUS fusion biopsies in local anesthesia without standard antibiotic prophylaxis – GUNZEL et al. WORLD JOURNAL OF UROLOGY, January 2021
- (3) Managing discordant findings between multiparametric resonance imaging and transrectal magnetic resonance imaging-directed prostate biopsy. The key role of magnetic resonance imaging-directed transperineal biopsy – BAJEAOT et al., European Urology Oncology, 2021
 United States
United States