Cognitive Fusion
Cognitive fusion is based on the experience of the urologist, who superimposes the MRI scans onto the ultrasound images “from memory” and in real-time. As the suspect areas detected during the MRI do not appear on the ultrasound images, precise targeting of the biopsies is not easily performed and leads to poor diagnosis.
Software Based Fusion
The use of MRI to detect prostate cancer represents the latest revolution in prostate cancer diagnosis. Until its development, ultrasound probes only were used for guidance, knowing they are limited to organ contour imaging, not the tumor inside of it.
Prostate fusion biopsy is a breakthrough technology made possible by overlaying ultrasound images of the prostate with MRI sequences for visualization and targeting lesions. Suspect areas detected by the MRI are thereby displayed on the ultrasound scanner, allowing the urologist to target the necessary biopsies in real-time.
The precise overlay (fusion) of MRI-ultrasound images is the first step essential to have a higher level of accuracy during the procedure. The fusion can be rigid or elastic.
In the case of “rigid” fusion, the MRI scans are simply superimposed onto the ultrasound images. Conversely, with “elastic” fusion, the MRI scans are superimposed and then automatically adjusted to better correspond to the contours of the ultrasound images, bringing this fusion to a higher level of accuracy.
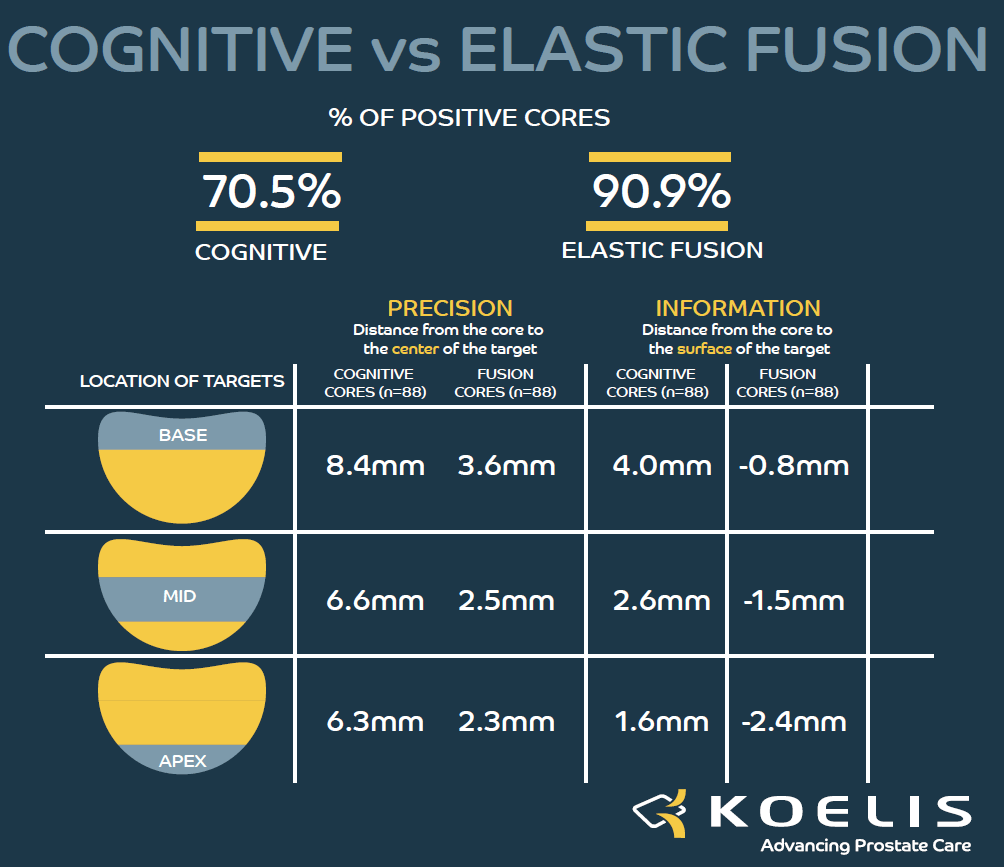
KOELIS Cognitive vs Elastic fusion
Today, aside from Koelis, all other fusion prostate biopsy systems use sensors (electromagnetic or robotic) to track the position of the ultrasound probe.Therefore, both lesion and core display are based on the probe location.
However, probe tracking systems do not compensate prostate deformation and patient movement.
These organ deformations or patient movements can be responsible for fusion misalignments between the MRI and ultrasound images. If not corrected, this results in a loss of accuracy in the MRI/ US fusion display which leads to inaccurate needle positioning on the prostate cartography, and, finally, to inaccurate biopsy precision.
KOELIS Probe Tracking
KOELIS has developed the only fusion technology that tracks the prostate itself, instead of the probe.
This approach to prostate diagnosis and care has significant benefits for clinical teams and patients eliminating the randomness of standard TRUS prostate biopsies.
Cognitive Fusion vs Software Based Fusion
This study measures the precision in the placement of a biopsy needle in a MRI target through MRI/TRUS fusion guidance using KOELIS OBT Fusion® technology compared to cognitive fusion.
Results: Cores obtained with the fusion technique achieved a higher precision than cores obtained from cognitive techniques 2.8 mm vs 7.1 mm. Fewer cancers were detected with the cognitive technique than with the fusion technique.
KOELIS® Technology for Fusion Biopsy
KOELIS OBT Explanation
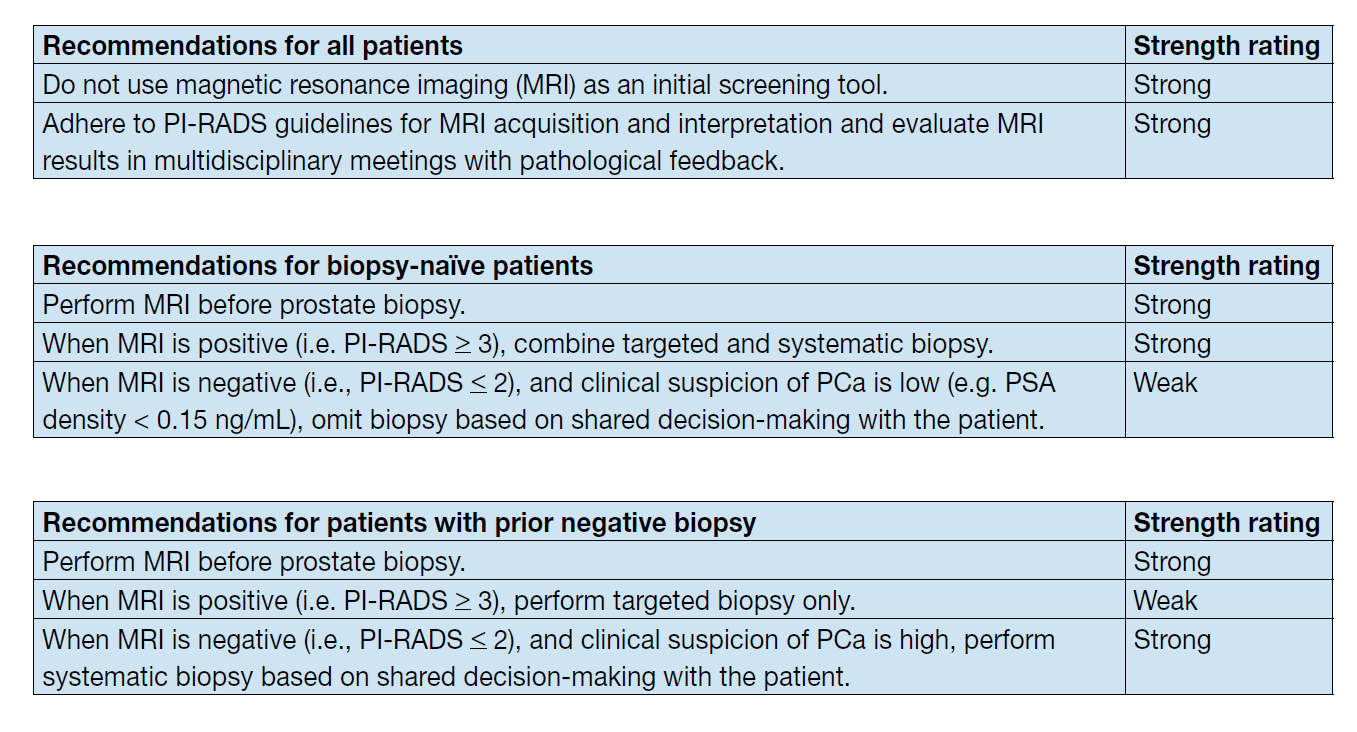
Guidelines
EAU Prostate Cancer Guidelines
The early use of multiparametric magnetic resonance imaging (mpMRI) before a prostate biopsy is recommended in both biopsy naïve patients and in patients with a prior negative biopsy for the detection of prostate cancer.
Publications:
- MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis – Veeru Kasivisvanathan et al. –New England Journal of Medicine – March 2018.
- Precision Matters in MR Imaging-targeted Prostate Biopsies: Evidence from a Prospective Study of Cognitive and Elastic Fusion Registration Transrectal Biopsies. Cornud et al. – Radiology – May 2018.
- Precision Matters in MR Imaging–targeted Prostate Biopsies: Evidence from a Prospective Study of Cognitive and Elastic Fusion Registration Transrectal Biopsies –Cornud et al. Radiology – May 2018
- Single-centre evaluation of systematic and targeted MRI biopsies for the diagnosis of prostate cancer – Lenfant et al. World Journal of Urology – 2022
 United States
United States