Active Surveillance
Active surveillance means not actively treating the cancer but rather monitoring the cancer progression over time through repeated diagnostic tests. Those regular assessments include PSA testing, MRI, Digital Rectal Examination (DRE), and biopsy. Due to its nature, active surveillance is an option for very low or low-risk prostate cancer.

To find out more about this technique and what KOELIS® technology can do, see our page on Active Surveillance.
Radical Prostatectomy
A radical prostatectomy is a surgical procedure in which the entire prostate is removed. It is a routine operation that can be performed using traditional techniques or with the assistance of a robot. Robotic surgery has been found to reduce post-operative pain and bleeding. However, the side effects remain similar to those of traditional surgery.

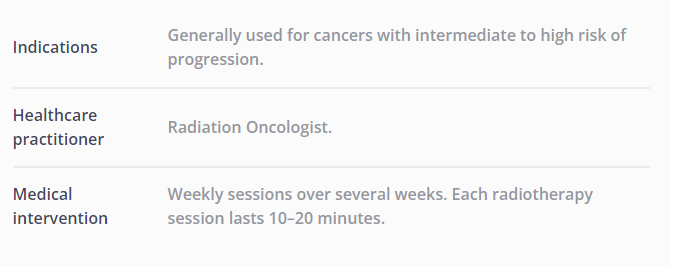
External Radiotherapy
In external radiotherapy, ionizing rays are aimed at the patient’s pelvis and focused on the prostate to irradiate the entire gland. The rays cause alterations in the DNA of the cancer cells, causing them to die. Radiotherapy protocols may involve a varying number of sessions depending on the treatment strategy and hospital equipment.
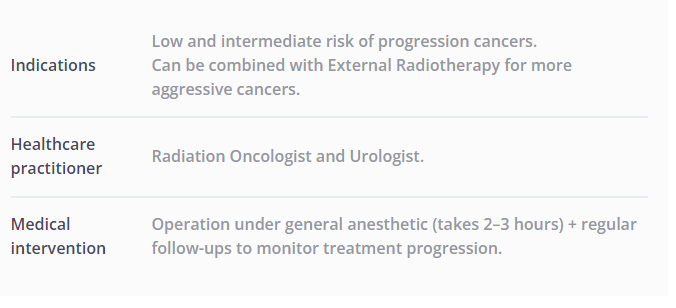
Internal Radiotherapy – Brachytherapy
Internal Radiotherapy, also known as Brachytherapy, is a treatment option where radioactive sources are inserted inside the prostate itself. These tiny sources (called seeds) are the size of a grain of rice and emit radiation within an area of a few millimeters. Typically, 60–100 seeds are used, depending on the cancer to be treated.
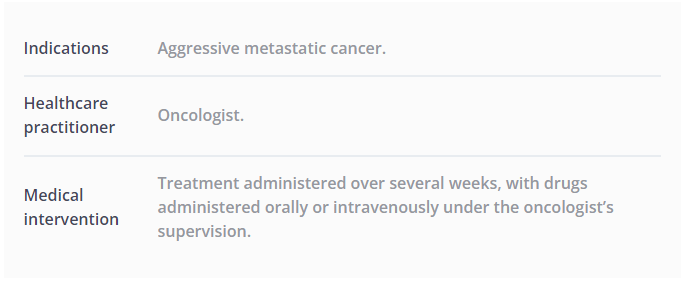
Chemotherapy
Chemotherapy is a treatment that is primarily recommended for advanced prostate cancers that have entered metastatic expansion. It halts cancer cells by preventing them from multiplying. It does not treat the cancer but rather limits its progression and aggressiveness. This means that chemotherapy is used alongside other more radical treatments that can altogether remove or destroy the tumor.
Alternative treatments
Newer techniques are being investigated to complement the existing range of treatment options. However, they are not recommended as widely as previous techniques by international urological societies. These procedures can either be whole-gland, i.e., the entire prostate can be treated, or subtotal (hemi-gland, or focal ablation).
The advantages of a subtotal ablation are that only the cancerous area of the prostate can be treated, leaving the healthy part untreated, thus better preserving urinary and erectile functions. However, subtotal or focal ablation is still undergoing clinical investigation and requires further clinical evidence before being implemented in the clinical guidelines.
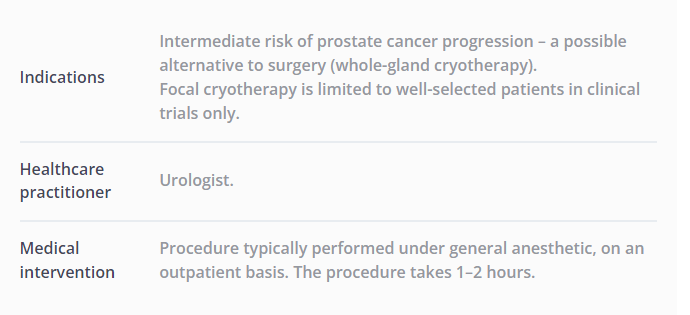
Cryotherapy
Cryotherapy is designed to kill cancer cells by freezing them below -40°C. To do this, cryoablation needles (generally 4-8) are inserted into the prostate transperineally. The needles produce cold, which destroys the cells while minimizing the impact on surrounding tissue and organs.
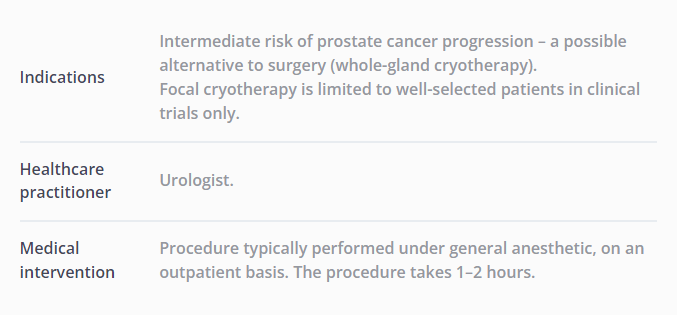
High-Intensity Focused Ultrasound (HIFU)
HIFU treatment uses high-intensity focused ultrasound to heat and kill cells at a temperature greater than 60°C. A dedicated ultrasound probe is inserted into the patient’s rectum, and the ultrasound emitted by this probe is focused on various areas of the prostate. As a result, there is a local increase in temperature, killing the cells. This local ablation is repeated at multiple angles and depths to produce an ablation covering the cancer area.
 United States
United States