Prostate biopsy is the only way to diagnose prostate cancer. It is always done under ultrasound guidance to visualize the prostate and the lesion. It exists two approaches: transrectal or transperineal. Today, transrectal approach is the most used by urologists from all around the world. To make the diagnosis more reliable, ultrasound images can be fused with MRI scans. For that, using a fusion system is necessary: it allows to fusion images for a better location of the lesions. This practice conquers more and more physicians. Is it the definition of modern urology?
Why switch to fusion system?
MRI and ultrasound fusion met success in the 90s for the staging of prostate cancer. However, the results were not always there. In the mid-2000s, a paradigm shift took place in the diagnostic and treatment of prostate cancer, when the notion of overtreatment was taken into consideration. MRI, first used to detect extra-prostatic tumors, has proven to be an effective tool for diagnosing prostate cancer. MRI makes possible to precisely locate the lesions, and thus, to better guide the biopsies. It is also proving to be a major ally for the post-treatment follow up of patients with prostate cancer.
Furthermore, MRI makes it possible to detect lesions in areas that are not easily accessible by biopsy, but also to rule out significant cancers. This makes it possible to better qualify the severity of the cancer and to adapt treatment accordingly (active surveillance or focal therapy instead of prostatectomy for example).
For more comfort of the patient, transperineal approach is preferred. This reduces the risk of infection, while improving detection rate. Unfortunately, only few doctors are trained for this practice, so it takes more time. The challenge is to equip center with devices and develop local anesthesia practice to build urology of tomorrow.
Some features about elastic fusion
- MRI before biopsy :
- 28% MRI negative: go on surveillance
- 72% MRI positive: go on targeted biopsy
- 28% unnecessary biopsies avoided
- MRI targeted biopsy:
- 46% more detection of significant cancer
- 56% less detection of insignificant cancer
- 3 time less biopsy cores
Source : https://koelis.com/academy/wp-content/uploads/KOELIS-infographics-KASIVIVANATHAN-2018.jpg
Expectations of a fusion system
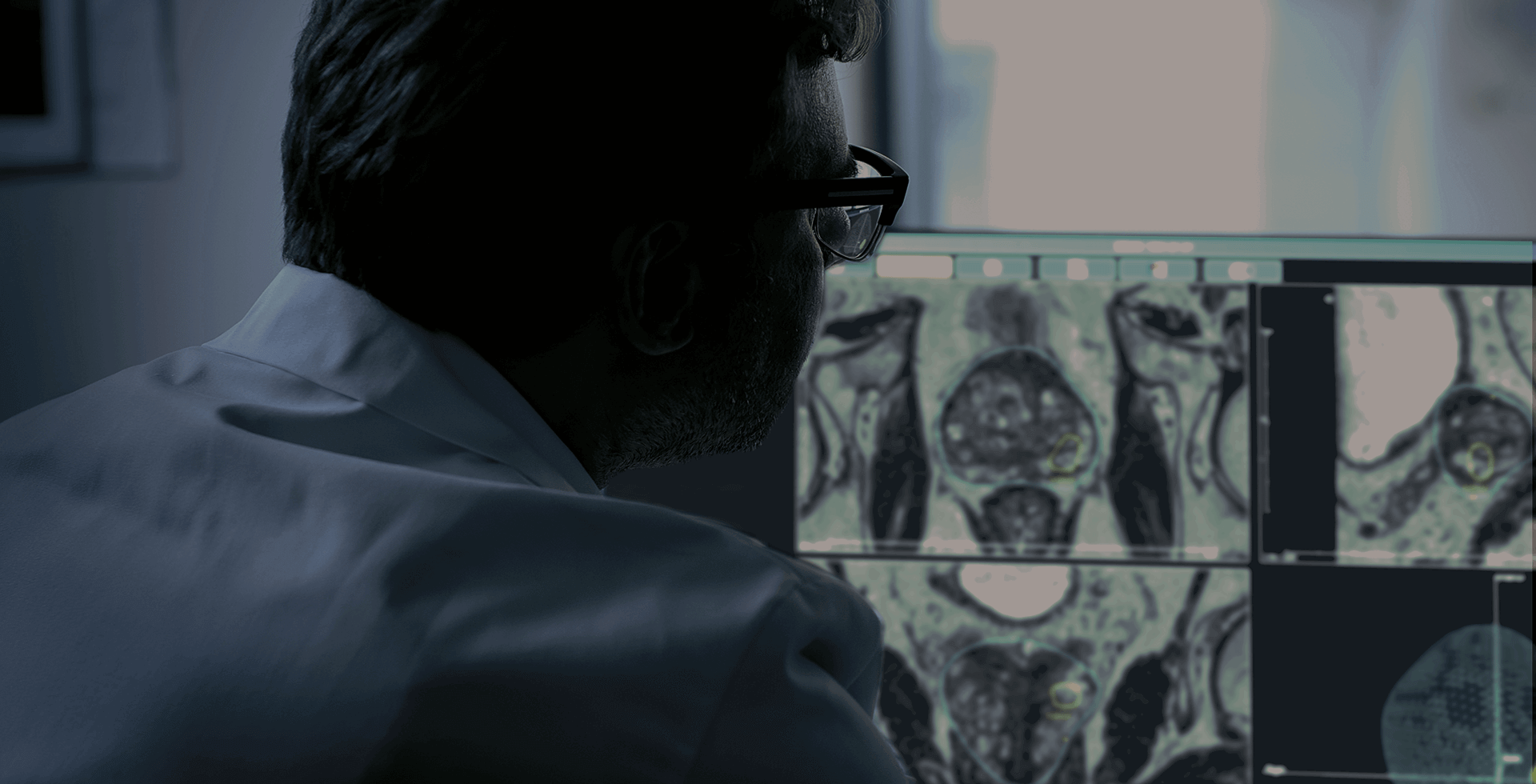
MRI/ultrasound fusion systems hold interesting promises. However, there are not all equal. Some features (functional or not) are therefore key to meet the expectations of physicians.
- Accuracy
Accuracy is key to effectively detect prostate lesions. The system must therefore be able to compensate for the movements of the patient and the prostate throughout the exam for an effective biopsy.
- Real time
To be precise, the urologist needs a real-time view of the prostate. It is the assurance of having successful targeted biopsies, thus making the diagnosis more reliable.
- Mobility
As we know, medical equipment can be bulky and difficult to transport from surgery room to another. A good fusion system must therefore be compact and mobile to be used by teams and to adapt to different medical establishments.
- Flexibility
Always with practicality in mind, the system must be flexible, adaptable to changes in the practice of urologists: be able to add or remove accessories, have software that is easy to use and scalable, switch from transrectal to transperineal approach, etc.
- The needle-guidance
The real advantage of fusion system is to offer a real-time view with needle-guidance and sample marking. It is a real help for urologists who can thus focus on the exam, while not questioning its reliability.
- Documentation available
Of course, all medical systems are effective when you know how to use them. And for that, the available training and instructions are key. Documentation is therefore essential to democratize the use of fusion systems.
The benefits of the Koelis’ fusion system: Trinity®
Trinity® by Koelis is a all-in-one fusion system. It is made to fit your clinic. Mobile, ultrasound system integrated and without any extra instrumentation, Koelis Trinity® incorporates into any clinical practices. The 3D probes (rectal and perineal) are adapted to the fusion system. They are manufactured to fit the OBT® technology and to give accuracy to physicians’ diagnostics. Finally, the patented organ-based® technology identifies and compensates for patient movements and prostate deformations. It records each core location with millimetric accuracy. It is performed automatically at each biopsy. It works only with our 3D probes. These are what makes us quite unique.
The transperineal MRI/ultrasound fusion helps physicians to trust their diagnostics, reduce number of biopsies, improve patient comfort and obtain good results and high detection rates, with low infection risk. Koelis Trinity® fits each practice (local or general anesthesia), so doctors can introduce it to the clinic easily, without any adjustment. To make this introduction a success, training is essential. If you want to know more about, don’t hesitate to contact us.
Sources :
- https://www.academia.edu/21890037/Pourquoi_et_comment_d%C3%A9tecter_le_cancer_de_la_prostate_en_IRM_
- https://koelis.com/academy/wp-content/uploads/KOELIS-Infographics-JACEWICZ-2020.pdf
- initial results of perineal MRI/ultrasound fusion biopsies under local anesthesia without standard perioperative antibiotic prophylaxis ;
- multicenter transperineal MRI-TRUS fuision guided outpatient clinic prostate biopsies under local anesthesia ;
- infection rate and complications after 621 transperineal MRI-TRUS fusion biopsies in local anethesia without standard antibiotic prophylaxis.
- Testimony of Dr Guntzel
 United States
United States