A prostate biopsy is the removal of tiny samples of prostate tissue to examine it for signs of prostate cancer.
Why the Test is Performed?
A prostate biopsy is the only medical procedure with which prostate cancer can be diagnosed conclusively.
Your doctor may recommend a prostate biopsy if:
- A blood test shows that you have a higher-than-normal prostate specific antigen (PSA) level.
- Your doctors discover a lump or abnormality in your prostate during a digital rectal exam.
How to Prepare for the Test?
Your doctor will inform you about the risks and benefits of the biopsy.
Several days before the biopsy, your doctor may tell you to stop taking any anticoagulants, NSAIDs, such as aspirin and ibuprofen, herbal supplements, vitamins.
Continue to take any prescription medicines unless your doctor tells you not to take them.
How the biopsy is Performed?
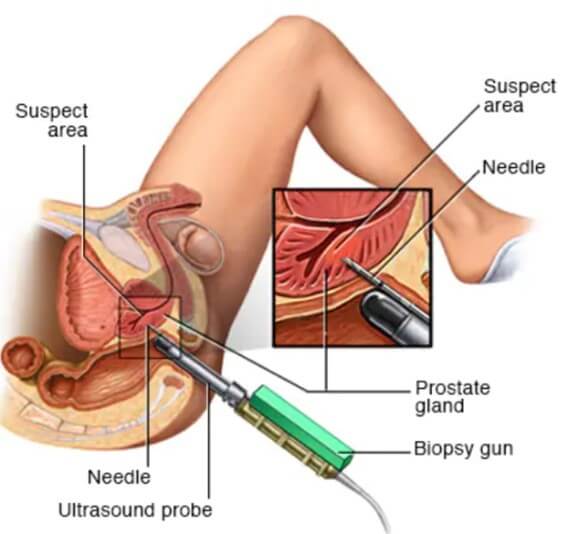
During the prostate biopsy procedure, the sampling needle may be inserted via the rectum (transrectal biopsy) or through the perineum (transperineal biopsy) under local or general anesthesia. In order guide the needle inside the prostate, endorectal ultrasound probe is inserted into the rectum.
The decision will be made by the doctor in consultation with the patient. A particular technique may be favored according to the patient’s wishes, the doctor’s experience, the location of the necessary biopsies and the available medical equipment.
A new accurate technique, the software fusion biopsy
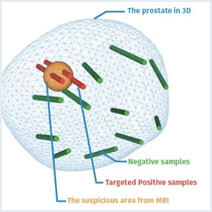
The development of the fusion of MRI images (interpreted by a specialist radiologist) and ultrasound images in live has revolutionized biopsy procedures. The urologist is now able to:
- Detect potential cancer sites before carrying out the biopsy thanks to MRI test.
- Locate suspect areas on the ultrasound image in real time during the biopsy.
- Guide the biopsy needle directly into the suspect areas on the MRI.
- Record the position of the biopsies performed in 3D prostate mapping (information that is essential for diagnosis and follow-up).
- Targeted precision of a few millimeters
The KOELIS Trinity® has set a new prostate biopsy standard for accuracy and reliability in fusion prostate biopsies. It is the system of choice in many top centers around the world.
Post-biopsy results
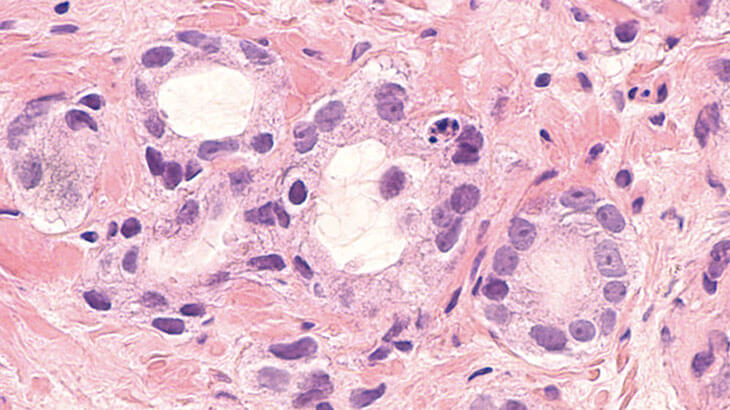
Once the prostate biopsy is complete, the samples taken are sent to a doctor specializing in the analysis of cancer cells: the anatomical pathologist.
This specialist will then determine whether or not cancer tissue is present in each sample. Any cancer cells are identified and classified according to their aggressiveness and size using a Gleason Score.
Normal Results
Normal results from the biopsy suggest that no cancer cells have been found.
What Abnormal Results Mean?
A positive biopsy result means that cancer cells have been found. The lab will give the cells a grade called a Gleason score. This helps predict how fast the cancer will grow. Your doctor will talk to you about your treatment options.
The biopsy may also show cells that look abnormal but may or may not be cancer. Your provider will talk with you about what steps to take. You may need another biopsy.
Example of results: A detailed diagnosis in a KOELIS Trinity 3D mapping leading to personalized patient care.
What are the risks? Complications and side effects?
The primary complications during the prostate biopsy procedure are very much related to the anaesthesia. A prostate biopsy generally takes place without consequence, yet side effects may be observed:
- Pain and discomfort around the sampled area(s)
- Difficulty urinating
- Bleeding of the prostate – Presence of blood in urine/sperm
- Side effects due to general anaesthetic
- Risk of infection (lower for transperineal biopsy)
 United States
United States