The most common eligibility criteria for this strategy are:
- Gleason Grade 3+3 (equivalent to ISUP Grade Group 1)
- Clinical stage cT1c or cT2a
- PSA < 10 ng/mL
In recent cohorts, active surveillance has shown to be a viable approach for well-selected patients with a Gleason Grade 3+4 (ISUP 2). Eligibility for an active surveillance program must be discussed individually with a certified urologist. As a medium to long-term strategy, this management system involves monitoring cancer development with regular PSA testing, MRI, and biopsies. Active treatment can be initiated in the case of cancer progression or if the patient’s perceived risk/benefit ratio changes over time.
Advantages of active surveillance
- Avoid or delay the side effects commonly associated with active treatment (erectile dysfunction, urinary incontinence, bowel dysfunction, etc.)
- No risk or inconvenience associated with an operating room intervention (general anesthesia, recovery after the procedure, scarring, etc.)
- No compromise of the cancer control that can be treated in the case of progression
Disadvantages of active surveillance
- Risk of uncontrolled cancer progression that may alter the treatment efficacy. However, several studies have found that this risk remains very low for eligible patients.
- Regular prostate biopsies, increasing the discomfort linked to this procedure and the potential risk of sepsis (especially for repeat transrectal-guided biopsies)
- Increased number of follow-up tests during the monitoring period (regular MRI, PSA testing, and biopsies)
- Anxiety due to the nature of surveillance, which does not treat the cancer that is present in the organ
Watchful waiting
Watchful waiting is a management strategy similar to active surveillance. The main difference is that fewer or no follow-up diagnostic tests are performed in a watchful waiting program. Consequently, the side-effects linked to repeated biopsies are reduced if this procedure is removed from the monitoring plan.
Conversely, in the case of cancer progression, it may not be detected or may be detected less quickly than in an active surveillance program.
For this reason, watchful waiting is often recommended for patients whose life expectancy is < 10 years and who are at risk of dying from a cause other than prostate cancer, while preserving their quality of life by avoiding any treatment or diagnosis-related side-effects.
Another difference between watchful waiting and active surveillance is that watchful waiting can be offered to patients with higher-risk prostate cancer (intermediate or high), provided that the benefits/risk ratio related to life expectancy is preserved.
How KOELIS® technology enables better active surveillance?
For over a decade, KOELIS® has developed 3D imaging technologies to better diagnose, visualize and monitor prostate cancer. Our latest platform, KOELIS Trinity®, integrates all of these technologies into an intelligent, intuitive, and efficient workflow that can benefit all patients at risk of prostate cancer.
The efficacy of an active surveillance program lies in the quality of the cancer stage monitoring. Namely, repeated follow-up biopsies at defined time intervals are the cornerstone of this strategy to track disease progression: if the Gleason score changes or if the size of the cancer measured on the biopsy cores progresses.
The standard practice for active surveillance biopsy is 12 systematic transrectally or transperineally guided cores in random areas of the prostate to identify the potential cancer foci (Figure 1).
Figure 1: Standard scheme for 12 cores systematic biopsy
The major drawbacks of this conventional approach are:
- These biopsies are performed with 2D Ultrasound, leading to heterogeneous sampling of the prostate due to the difficulty for the physician to cognitively image the organ in 3D. This heterogeneous sampling can lead to large areas of the prostate remaining unsampled.
- The locations of the biopsy cores are not recorded from one biopsy exam to another. It is, therefore, impossible for the physician to know precisely whether follow-up biopsies have been taken in exactly the same place as before and thus whether the stage of the cancer in a previous positive core has evolved or not.
KOELIS Trinity® solves both of these issues while helping physicians choose the best management strategy for each patient:
- All biopsy core locations and spatial coordinates are stored in the KOELIS Trinity® system for all biopsy examinations (not only those for active surveillance). This 3D model (Figure 2) generated specifically for each patient allows physicians to review a patient’s case at any time.
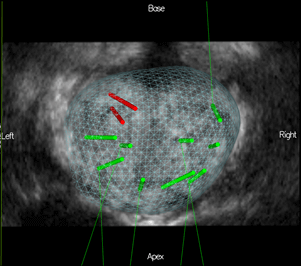 Figure 2: 3D prostate map after a systematic biopsy exam, where 2 cores are positive for cancer (red)
Figure 2: 3D prostate map after a systematic biopsy exam, where 2 cores are positive for cancer (red)
- At the time of re-biopsy, the physician can review the patient’s previous record and recall all information in the newest biopsy exam. Therefore, this KOELIS Trinity® 2nd Look technology allows for re-biopsy of previous positive areas but also allows for the sampling of areas of the prostate that may have been left unsampled during the previous examination (see Figure 3).
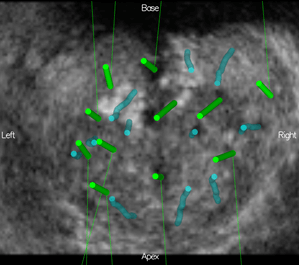 Figure 3: 3D prostate map after a second biopsy examination: previous negative cores are in blue (purple if positive), newest negative cores are in green (red if positive)
Figure 3: 3D prostate map after a second biopsy examination: previous negative cores are in blue (purple if positive), newest negative cores are in green (red if positive)
Additionally, the 2nd Look technology can be combined with other KOELIS Trinity® technologies such as MRI/US fusion (see Figure 4). This is in line with recent active surveillance protocols where repeated MRI can be performed in-between the biopsy examinations.
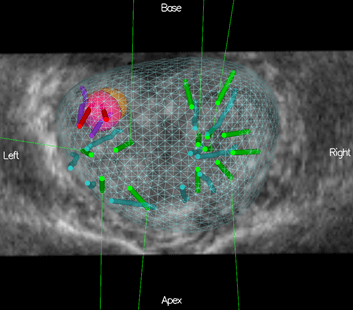
Figure 4: 3D prostate map after a second biopsy examination with MRI targets: the pink target was recalled from a previous MRI, the most recent MRI shows an orange target. Targeted and systematic cores were performed during the first and most recent (2nd Look) exam
For more information, contact us.
- The role of MRI in active surveillance for men with localized prostate cancer- Recabal P et al. Curr Opin Urol – November 2015
- Integrated US-MR fusion images and MR targeted biopsies. What are their role and value in the detection and follow-up of prostate cancer.- Delongchamps et al.Arch Esp Urol. April 2015
- A novel technique using three-dimensionally documented biopsy mapping allows precise re-visiting of prostate cancer foci with serial surveillance of cell cycle progression gene panel.Ukimura et al. –Prostate – June 2015
- Innovations in prostate biopsy strategies for active surveillance and focal therapy.Ukimura et al.-Curr Opin Urol – March 2011
 United States
United States